
March 15 was Match Day, and medical students across the country opened envelopes to learn which medical center and specialty they matched with for their residency training. For the first time in many years, there was a gap in the number of matches for radiation oncology with 29 slots going unfilled.
So why was there a gap in RO this year? Some believe this reflects an anticipated oversupply of radiation oncologists for the future. This concern appears to depend largely on geography, where some markets are showing limited job options and some markets much broader options. Some believe that these unmatched slots signal a concerning decline in the field. Others view the 2019 match as a simple market correction. Many have asked, what could, or should ASTRO or others have done to prevent this? It is important to note that there is no single oversight entity that controls the number of residency slots in a field, and anti-trust laws prohibit organizations such as ASTRO from engaging in activities that could negatively impact the U.S. free marketplace.
There were several preview signs that the specialty could experience this type of Match Day with several factors at play. As a first step, it may be valuable to review the overall resident training and oversight ecosystem. Each player has an integral role in the health of a system that trains a medical student to provide specialized care as a licensed physician.
Association of American Medical Colleges (AAMC): The not-for-profit association whose members include medical schools and teaching hospitals. They help students navigate the journey from pre-med through residency. Because their members include all the accredited medical schools, they manage the national residency matching program (NRMP) which occurred last week. They frequently advocate for federal funding for graduate medical education.
Medicare Program and Graduate Medical Education: In addition to setting the reimbursement rates it will pay for services for Medicare beneficiaries, Medicare recognizes that hospitals who train residents incur real and significant costs beyond those customarily associated with providing patient care. The Medicare program makes payments to teaching hospitals for a portion of these added costs through direct graduate medical education (DGME) payments. The DGME payment compensates teaching hospitals for "Medicare's share" of the costs directly related to the training of residents.
Accreditation Council for Graduate Medical Education (ACGME): The ACGME is an independent, not-for-profit, physician-led organization that sets and monitors the professional educational standards for residency programs. The ACMGE is responsible for defining the residency requirements for each specialty and has review committees for each specialty and fellowship area. The ACGME also has a process to evaluate, improve, and publicly recognize institutions and programs in GME that are in substantial compliance with standards of educational quality established by the ACGME. Lastly, the ACGME manages the case report system residents use to demonstrate progress toward requirements outlined in the residency requirements.
Teaching Hospitals: While Medicare controls how much it will pay per resident to a teaching hospital, a hospital may use its own money to fund additional residents. Each individual hospital decides if it would like to dedicate any of its own funds for this purpose and if so, how much and on which areas it would like to expand its training programs. Thus, the total number of residency slots in any specialty in a year is the sum of each individual teaching hospital’s decision about how many slots it will offer.
While GME funding has been flat since 1997, the number of radiation oncology programs and the number of residency slots has grown over the last decade. As you can see in this chart, both the number of programs and the number of slots offered by programs has expanded over the last decade.
Radiation Oncology Residency: 2006-2018 trends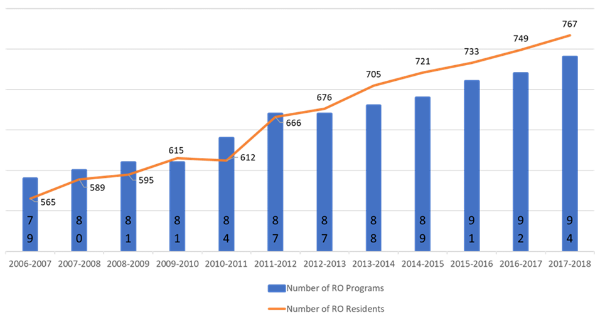
Source: ACGME Data Resource Books
Upon completion of residency training, physicians then prepare for board examinations. In radiation oncology, the American Board of Radiology is the board which designs and tests individuals as to their competency in the practice of radiation oncology. They require individuals to pass three examinations to receive board certification: clinical, (radio)biology and medical physics. Boards also have various requirements to maintain certification that physicians must meet defined by the American Board of Medical Specialties.
Once a medical student or resident identifies their preferred specialty, they often join an affiliated specialty society to begin networking and become a member of the community. ASTRO is the membership organization with members defined as board certified radiation oncologists and medical physicists. ASTRO's role is to provide leadership to help guide the specialty into the future. ASTRO is dedicated to improving patient care and our core priorities including continuing professional education and training and the advancement of quality improvement, science and advocacy.
With regard to the workforce of radiation oncologists, ASTRO regularly studies and identifies trends through surveys and research. ASTRO's scientific journals also publish studies done by others about our workforce, including this 2016 study that predicted that current training program numbers could lead to an oversupply. These forecasts use predominantly historic information and often fail to capture how new scientific discovery and innovation might create new possibilities for the field. Still, it is important that these forecasts be available for medical students so that as they consider their future, they can make informed decisions about which field(s) they wish to pursue.
ASTRO can and does advocate for the modernization of training requirements to prepare radiation oncologists for the future. We anticipate that the ACGME will soon release a proposal to update the radiation oncology residency program requirements, and we will use this as an opportunity to comment with an eye toward the future health and growth of the specialty.
A 2019 ASTRO survey identifies that practicing radiation oncologists are most passionate about patient care interactions and being able to participate in the cure of cancer. Radiation oncology remains a critical modality of cancer treatment for patients around the world. The 2019 Match Day results will trigger highly welcome discourse about the specialty and the residency training landscape. ASTRO will do everything we can to help facilitate discussion and the sharing of accurate information.


