RO-ILS Participation
RO-ILS participation benefits both patients and staff. The more integrated RO-ILS is into a practice, the better the local learning opportunities and possibilities for improvement, leading to superior outcomes and an empowered staff culture.
 "As our team has adopted and participated more in the RO-ILS event submission process, our team has become more cohesive and higher-performing. There has been a psychological shift over the past few years because of our RO-ILS participation." — John Ready, PhD, DABR Sutter Medical Foundation Read an interview with Dr. Ready |
Practices also have the ability to impact the broader radiation oncology community by reporting to the PSO. Data in each practice's local RO-ILS Portal is not automatically in the aggregate RO-ILS database. Easy, secure reporting to the RO-ILS database enables the practice’s data to have a better impact. Comprehensive, de-identified RO-ILS education based on aggregated RO-ILS data helps identify trends and mitigate errors for the entire radiation oncology field.
During RO-ILS enrollment , practices set up the following:
- RO-ILS Portal: The online platform that is used to enter, review and analyze data. For extra security, each practice has a unique URL to the RO-ILS Portal, managed by Clarity.
- Submitter Account: A general login to submit events into the RO-ILS Portal. This login is shared with all practice staff as it enables anonymous submission of safety events.
- Reviewer Accounts: Designated practice staff responsible for completing event review and reporting to the PSO. Reviewers have access to the practice’s RO-ILS data and often actively direct the practice’s patient safety activities. Each Reviewer has an individual login, and their activity is tracked in the Portal.
Participation in RO-ILS is based on the collection and analysis of patient safety data. The standard RO-ILS event reporting process consists of four steps.
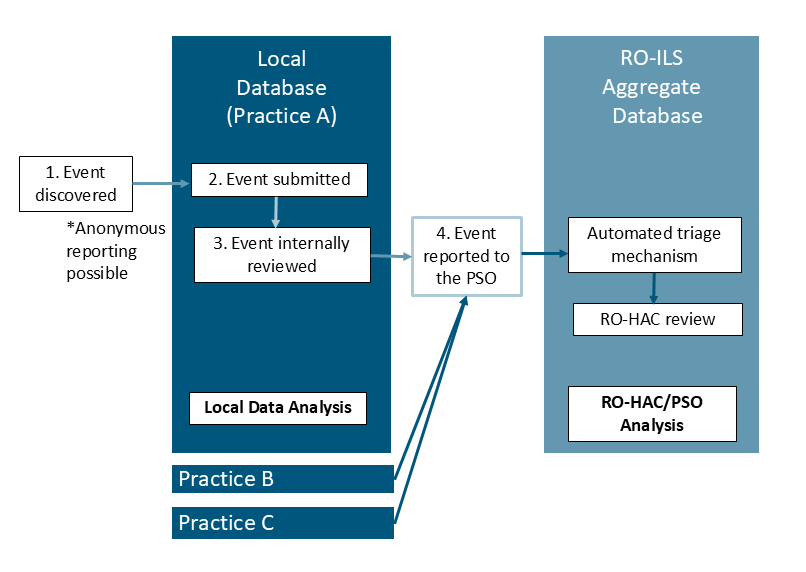
1. Event discovered
- RO-ILS accepts a variety of events. Events are classified as incidents that reach the patient (with or without harm), near misses, unsafe conditions, or operational/process improvement issues.
2. Event submitted
- Any staff member may log in to the practice’s unique RO-ILS Portal using the shared Submitter account and complete a brief “Submit Event” form.
3. Event internally reviewed
- Reviewer(s) receive an automatic notification of event submissions. Reviewer(s) may need to investigate the event per the practice’s internal protocol which can vary depending on the severity of the event. When ready, Reviewer(s) answer additional detailed questions in the “My Review” section of the Portal.
4. Event reported to the PSO
- A Reviewer must actively indicate that the event should be reported to the PSO via a dedicated data element in “My Review."
- If “yes” is selected, a copy of the event is shared with the aggregate RO-ILS database managed by the PSO. Any changes to the event in the local database will automatically be updated in the RO-ILS database.
- If “no” is selected, the event remains only in the local database and cannot have a wider impact for shared learning.
To be considered actively participating in RO-ILS, events must be reviewed and reported to the PSO, actions that can only be completed by Reviewers.
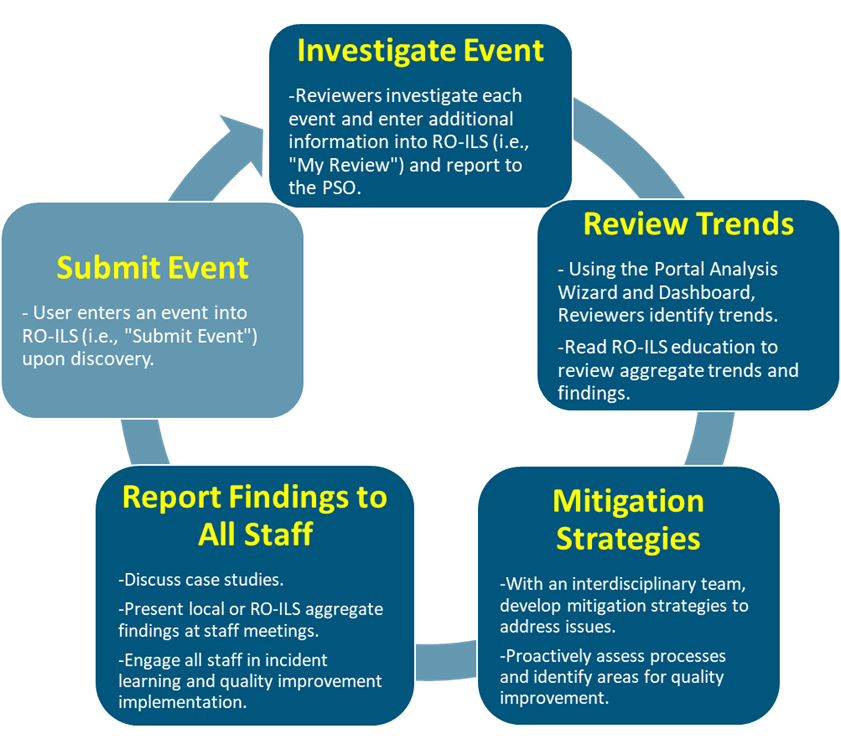
Incident learning is not a one-time event but should be viewed as a cyclical activity. Once data is properly collected, trends can identify weak processes that require attention or error pathways that need mitigation. When staff feel their concerns are heard and see issues being addressed, it creates a positive feedback loop that fosters more reporting and engagement. The image below includes examples of how RO-ILS data can be used internally to strengthen and sustain a robust culture of continuous learning.
Enrolled practices should consider the following topics that can affect participation.
- Safety culture: For optimal learning and active RO-ILS participation, practices need a strong culture and building and maintaining a culture of safety requires ongoing attention. Incident learning is about identifying mechanisms to minimize error pathways, not about punishing staff. Staff should feel safe reporting events and understand there will be no retribution for doing so. When investigating the event, focus on the process and structural factors that contributed to the event and not blaming the person. Pay attention to tone and word choice when discussing events as this can deter staff engagement. To improve transparency, share RO-ILS processes and involve all staff in identifying mitigation strategies. Consider assessing the safety culture with a formal tool and address areas for improvement.
- Platform familiarity: It is essential for practices to identify and remove barriers to submission. Staff need to feel comfortable accessing and submitting an event in the RO-ILS Portal so practices should regularly re-educate existing and new staff on how to enter an event into RO-ILS using the resources provided. For example, once a quarter, play the RO-ILS submission training video at an all-staff meeting or enter an event in real time.
- Analysis: The RO-ILS Portal has many built-in tools to assist with trending data. The Dashboard features six live, preset graphs that provide immediate insights into key data elements, making it easier for staff to understand and engage with their data. While it may seem counterintuitive, more reporting, especially a higher ratio of near misses to actual incidents, is associated with safer practices. Therefore, tracking trends in reporting is helpful as an engagement metric that can easily be achieved with the RO-ILS Dashboard. Reviewers can also use the AnalysisWizard to create custom reports with any RO-ILS data element, allowing for tailored output to meet their specific needs. Practices can save templates for future use and set up automated, recurring reports, streamlining the report development process and fostering a proactive and engaged approach to incident learning to share with staff. On a regular basis, share local data trends with all staff using the RO-ILS Dashboard orAnalysisWizard reports.
- Encouragement: Practices should identify ways to celebrate staff for catching errors and encourage reporting. For example, this could be recognizing staff with a “great catch” award throughout the year and/or during Patient Safety Awareness Week. Consider nominating a staff member for national recognition as a Safety Star.
- Focus areas: Practices may want to emphasize a specific topic for quality improvement and promote submission of events in this area. By selecting a focus area (e.g., imaging, simulation), staff may be more hypervigilant in identifying and submitting issues previously glossed over. This helps staff build a habit of reporting that will hopefully extend beyond the focus areas.
- Expanded use: While “incident” is specified in the RO-ILS name, the program collects a wider range of events. The event classification program document provides examples of “operational/process improvement” events that can be tracked such as patient complaints and severe patient outcomes warranting discussion at a morbidity and mortality conference. Additionally, the RO-ILS Portal can be used as a tool to track DEI-related events impacting, or with the potential to impact, patient safety. This can help the practice take action to create a safer, more inclusive work environment for staff and improved health care experience for patients. A program resource, spearheaded by ASTRO’s Leadership Pathway Program awardee, includes background information and examples of DEI-associated safety events and recommendations on how it could be tracked in RO-ILS.
For support or to learn more, please email the ROILS staff.


