Radiopharmaceutical therapy offers promise for people with tough-to-treat meningioma brain tumors
Phase 2 clinical trial finds 177Lu-Dotatate may extend progression-free survival for patients with no other options to manage recurrent disease
WASHINGTON, September 29, 2024
A radiopharmaceutical therapy that has successfully extended progression-free survival for patients with neuroendocrine tumors shows early promise for delivering similar benefits to patients with difficult-to-treat meningioma, a type of brain tumor. Findings of the nonrandomized phase II study will be presented today at the American Society for Radiation Oncology (ASTRO) Annual Meeting.
“We’ve found a therapy with a meaningful signal for effectiveness and safety for people with refractory meningioma, a condition with no standard treatment options,” said Kenneth W. Merrell, MD, principal investigator (PI) of the trial and a radiation oncologist at the Mayo Clinic Alix School of Medicine in Rochester, Minn.
“Nearly 80% of patients in our study were progression-free after six months. This rate greatly surpassed the benchmark from prior research, suggesting that radiopharmaceuticals are a promising therapeutic agent for these patients.”
Meningiomas are tumors that grow in the connective tissue surrounding the brain and spinal cord. They are the most common type of primary brain tumor, and while they typically do not spread to other parts of the body, they can grow uncontrollably and lead to disabling and deadly compression of the nerves and brain.
Standard treatment for patients with meningiomas is either surgical removal or external beam radiation therapy when tumors grow in areas where surgery is too dangerous, such as close to the brain stem or spinal cord. But for the portion of patients where the tumor grows despite these treatments, known as refractory meningioma, the tumors tend to behave more aggressively, and retreatment is difficult because radiation and surgery cannot be repeated frequently without greater risks.
“There is no standard of care or proven option for managing refractory meningioma. Many of these patients continue to experience aggressive tumor growth and significant related complications, and ultimately the illness may prove fatal. It is a very challenging prognosis to manage, and in many cases, we are left with only supportive measures,” Dr. Merrell said.
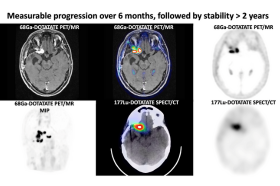
Dr. Merrell and his colleagues investigated whether patients with refractory meningioma would benefit from theranostics, an approach that combines therapy with diagnostics for personalized internal delivery of radiation treatment. Theranostics leverages radiopharmaceuticals — specialized medicine containing radioactive material — to find cancer cells in the body and attack them with precise doses of radiation, without harming the surrounding healthy tissue. This dual-pronged approach offers patients a more tailored, and potentially more effective, treatment option.
While still an emerging treatment modality, radiopharmaceuticals are commonly used to treat thyroid cancer, metastatic cancer such as bone metastases from prostate cancer, and other types of tumors. For this trial, researchers looked specifically at 177Lu-Dotatate, an FDA-approved radiopharmaceutical for neuroendocrine tumors, which share biological similarities with meningiomas.
“There have been many attempts at testing a variety of chemotherapies and other systemic agents for these patients. And others have looked at this option for therapy, but no one had completed a prospective trial for this patient population before ours,” said Geoffrey B. Johnson, MD, PhD, the co-PI of the trial and a nuclear medicine physician at the Mayo Clinic.
“With advanced PET imaging, the theranostic approach to treatment helps us to select those patients most likely to benefit from molecularly targeted radiation directly to their tumor cells.”
The researchers conducted a single-arm, phase II clinical trial at a large academic center, enrolling patients with refractory meningioma that had grown at a rate of 15% or more over a six-month period. During a three-year period beginning in April 2020, patients including 20 people with WHO grade 2 or 3 disease were enrolled into the study. The median patient age was 67, and nearly all (95%) had grade 2 meningiomas. Trial participants received four infusions of 177Lu-Dotatate spaced eight weeks apart.
Six months after treatment, 78% of patients had not experienced further tumor progression, far exceeding the benchmark progression-free survival rate of 26% established by prior research. The median time before patients’ cancer progressed was 11.5 months.
After one year, overall survival was 88.9%. No patients experienced life-threatening side effects, while 10 had severely low blood counts, one had grade 3 hepatitis and one had a grade 3 seizure possibly related to treatment. Five patients did not complete treatment due to tumor progression (n=2), adverse events possibly related to treatment (n=2) or other comorbidities (n-1).
“Most patients tolerated the treatment well,” Dr. Merrell said. “It appears that 177Lu-Dotatate is a safe and rational therapeutic choice with broad eligibility for patients with aggressively growing meningiomas, particularly as alternative therapy options are limited.”
“As there is no current standard of care for these patients, our findings establish a new benchmark and may influence the treatment options available.”
###
This press release contains updated findings/data from the study authors.
Attribution to the American Society for Radiation Oncology (ASTRO) Annual Meeting is requested in all coverage.
Study/Presentation Details
- Abstract 2: A prospective, phase II study of 177Lu-Dotatate in patients with surgery- and radiation- refractory meningioma: Results of the WHO grade II/III cohort (View here.)
- News Briefing: Tuesday, October 1, 9:00 a.m. Eastern time. View details. Register.
- Scientific Presentation: Sunday, September 29, 1:00 p.m. Eastern time, Walter E. Washington Convention Center. Email ASTRO's press team to access the livestream or recording.
- This was an investigator initiated clinical trial, with funding to support from Novartis.
ABOUT ASTRO
The American Society for Radiation Oncology (ASTRO) is the largest radiation oncology society in the world, with more than 10,000 members who are physicians, nurses, biologists, physicists, radiation therapists, dosimetrists and other health care professionals who specialize in treating patients with radiation therapies. Radiation therapy contributes to 40% of global cancer cures, and more than a million Americans receive radiation treatments for cancer each year. For information on radiation therapy, visit RTAnswers.org. To learn more about ASTRO, visit our website and follow us on social media.


